Dental Decay & Treatment
What is Tooth Decay?
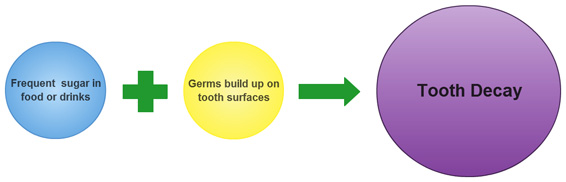
Tooth decay is a process where acid made by bacteria (germs) attacks the tooth surface and gradually causes a cavity (hole). Acid is made by bacteria when sugary food or drink items are consumed frequently.
So a combination of germs, sugars and the pattern in which they combine in your mouth causes the problem.
Tooth decay is very common in Ireland across all age groups. Despite great advances in the type of dentistry we provide, at the end of the day, we want to help you avoid needing these treatments. This means listening to preventative advice and putting it into action every day at home.
Is tooth decay preventable?
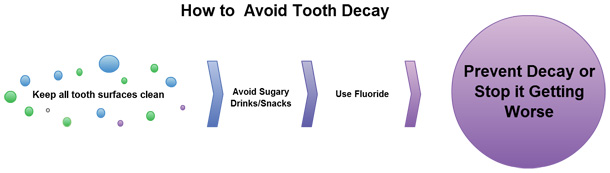
Yes, it is completely preventable! If you make sure you follow Three Key Steps:
- 1. Keep all tooth surfaces clean by brushing thoroughly twice a day and flossing once a day.
- 2. Keep the amount and frequency of eating or drinking sugary items to a minimum. Between meals snacking on anything containing sugar in particular should be avoided. Have a detailed look at what you eat and drink and how often you eat them. Doing a diet sheet for a few days is a great way to highlight the frequency with which you eat less healthy items. Click here for a printable diet sheet. Fill it up and bring it along for your check-up and we'll help you with it.
- 3. Use fluoride toothpaste (preferably with at least 1000ppm sodium fluoride- look at the ingredients on the back of the tube) and maybe a fluoride mouthwash also. Fluoride strengthens the enamel surface, making it more resistant to acid. Don't rinse vigorously with water after brushing; spit out excess toothpaste only. The fluoride then has a chance to work on strengthening the tooth surfaces.
So Big Deal if I need a filling - everyone has them - what's the problem?
A filling only fills a hole in your tooth. That tooth is then weaker and more likely to need other treatment for the rest of your life. The average filling lasts about 10-15 years, meaning if you get a filling done at age 15 years, you may have to replace that filling 4-5 times during your life. Each time it's replaced it gets a little bigger and the tooth gets a little weaker- often eventually leading to more complicated dentistry like root canal treatments and crowns or tooth removal. By avoiding the need for that treatment in the first place, you avoid all that dental treatment throughout your life. This is especially important for teenagers and young adults to understand….what you do now to take care of your teeth will decide the condition of your teeth when you are 30, 40, 50, 60, 70, 80 years old and how much of your hard-earned cash you have to spend on them!
Will I see one of these cavities in my mouth?
 |
 |
 |
| The brown spot and shadow on this tooth indicate there is decay underneath. | The cavity is much larger than it first appeared. The brown dentine is soft and full of bacteria so is removed. | The tooth is restored with a white composite filling. The green cover is a rubber dam used to keep the tooth clean and dry during the treatment. |
Tooth decay starts on the outer surface of the tooth (enamel). The germs penetrate to the next layer (dentine) and most of the structural damage occurs here. However the enamel often stays intact until the cavity is quite large so it is not visible to the untrained eye. Even when you visit the dentist, a cavity may not show up until xrays are taken. This is why attending the dentist regularly for a health check is so important. At Oranmore Dental Care, we recommend that everyone visit for a check up at least every 12 months and sometimes every 6 months. This enables us to detect problems early before they cause pain or infection.
So if you can see a hole in your tooth, it's likely to be quite large and need attention ASAP.
Does tooth decay cause pain?
The level of pain you get from a dental cavity (hole) depends on how far the germs have travelled through the tooth. Tooth decay on enamel does not cause pain. Even a small to moderate sized cavity in dentine is usually not painful . As the germs gradually damage the dentine and move closer to the pulp (nerve) of the tooth, some discomfort may start. A typical example would be an area of your mouth becoming sensitive to sweet things and then to cold, lasting just a few seconds.
If the pain becomes more sharp or achy and last more than a couple of minutes, this is a sign of damage to the pulp by the bacteria. Unfortunately, your tooth may then require more advanced dental treatments like a root canal treatment or even extraction.
How long does it take for a cavity to develop?
From its starting point, as a chalky-looking white spot on the tooth surface to the point where the enamel surface is broken takes up to two years to develop. Therefore if you attend the dentist regularly - (at least once a year), you will be aware if you have a tooth decay problem and can takes steps to stop it getting worse.
Tooth decay can be stopped by taking the prevention steps already mentioned. Once the combination of acid-making bacteria and sugar are removed from the mouth, the tooth surface can harden and 'remineralize' (minerals in your saliva and toothpaste strengthen the weakened surface) over many months. To the inexperienced eye, the appearance of the tooth may not change and the affected area can in fact darken in colour. You may look at some dark spots on your teeth and be concerned that they need a filling when in fact they are scars of previous tooth decay. If you are unsure, the best thing to do is get them checked. When you attend a dentist you trust over a number of years, he/she is able to monitor these kinds of areas over time and only take action if they deteriorate, thus avoiding unnecessary treatment.
Back to top
Tooth Wear & Treatment
There are different types of tooth wear and it is important to understand their causes:
- Tooth Erosion is caused by tooth contact with acid.
- Bruxism (grinding) is caused by you rubbing teeth against each other.
- Tooth Abrasion is caused by you rubbing something hard against your tooth, usually your toothbrush.
- Combinations of the above can occur causing very rapid loss of tooth structure and weakening of your teeth.
Tooth Erosion (Acid Damage)
This is a different problem to tooth decay though the two can combine to cause a lot of damage to your teeth. Tooth erosion is thinning of the enamel and dentine of a tooth caused by direct contact of acid against the surface. It is not caused by bacteria. As with tooth decay, once the tooth structure is gone, it does not return.
What acids cause tooth erosion?
Acidic foods/drinks are the main problem. These include all fizzy drinks, wine, fruit especially citrus, juices, smoothies sports drinks. The acid may also come from your stomach that is if you suffer from acid reflux (heartburn) or an eating disorder, anorexia or bulimia.
What teeth are affected?
Any teeth can be affected by acid damage but the teeth most commonly affected are your upper front teeth. This is because acidic drinks come in contact with the palatal (facing the palate) surface and your tongue rubs against that surface when you swallow. The tooth gradually thins and starts to look more 'see-through'. The edge is then more brittle and can chip easily making them look uneven. Because it affects your enamel which is the white part of your tooth, your teeth will also become more yellow in colour over time and are more difficult to whiten effectively.
OK, so if I have one of these drinks I'll brush my teeth straight after!
No, don't do that! If you brush your teeth when the surface is softened, you'll do more damage! The minerals in your saliva can do some repair work if you give them time. So Don't Brush straightaway….wait at least 30 minutes. Best of all, be sensible about how often you consume any of the food/drinks which cause the problem.
Tooth Grinding
Many people grind their teeth against each other, usually when asleep. The causes of this problem vary but have a close association with stress. The teeth rub hard against each there and eventually wear down causing flattened tooth edges and shorter looking teeth. Grinding can also cause pain in the muscles of the face and in the TMJ jaw joint.
If you notice that you tend to clench your teeth together or rub them against each other during the day, for example out of habit or when you are stressed, we advise that you make a big effort to break that habit. This can cause a lot of damage to your teeth by wearing them down and also creating tiny cracks in their structure, which can become bigger and cause tooth pieces to fracture off.
Breaking the habit of night-time grinding or clenching is more difficult because you are asleep. You cannot decide 'I won't grind my teeth to-night'! To protect your teeth from damage, we recommend you get a custom-made nightsplint made. This is like a small version of a sportsguard, worn to bed. It stops you grinding tooth on tooth and therefore you cannot do any damage.
Abrasion
This is wear on the side surfaces of your teeth, usually occurring close to the gumline and is most commonly associated with brushing excessively with a hard toothbrush. A soft toothbrush, used thoroughly and carefully, is more than adequate to remove any plaque and food debris present on your teeth. Continual use of a hard brush wears the sides of your teeth and should be avoided.
Back to top
Gum Disease & Treatment
Visiting the dentist is not all about 'getting a filling'. Maintaining the health of your gums is just as important as avoiding tooth decay.
What do healthy gums look like?

Healthy gums are pale pink in colour, look flat and come to definite point between the teeth. Healthy gums do not bleed. If your gums bleed when you brush close to the gumline, it is very likely that they are affected by some form of gum disease. If they have always bled when you brush close to the gumline, then you have probably always had some element of gum disease. You would not ignore inflammation in any other part of your body; your gums should be no different.
Gum disease can be divided into two categories: gingivitis and periodontitis.
Gingivitis
Gingivitis is inflammation of the gums caused by the presence of unfriendly bacteria (germs) at or below the gumline. These germs build up in a whitish coloured film over time when the area is not kept perfectly clean. This film is called plaque. When plaque is left sitting on the tooth surface it hardens and is then called tartar or calculus. With suitable treatment, gingivitis is fully reversible without damage to the structures supporting your teeth. Treatment consists of a thorough cleaning to remove all plaque and tartar, followed by improved oral hygiene by you. Sometimes suitable mouthwashes are also used to help kill the germs which cause the problem. Gingivitis can return quickly if you do not continue with those improved tooth-cleaning habits.
Periodontitis
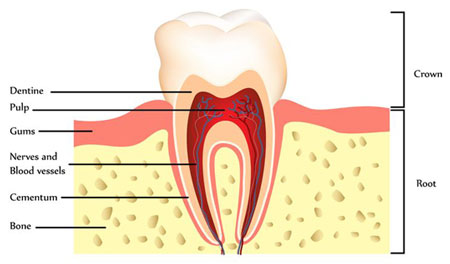
Periodontitis is inflammation of the gums and other tooth-supporting structures. It literally means 'around the tooth inflammation'.
- These supporting structures are:
- Bone
- Cementum (a cement on the root surface)
- Periodontal ligament ( a tiny ligament which connects cementum to bone)
- Gums
If you lose bone, cementum and periodontal ligament from around your teeth, it cannot grow back even if treatment is successful, i.e. the condition is treatable but the structural damage is irreversible. Even though the presence of plaque and tartar is the main cause of gum disease there are other factors which must be considered also.
Even though the presence of plaque and tartar is the main cause of gum disease there are other factors which must be considered also.
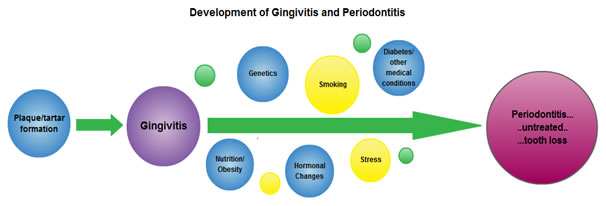
1. Genetics
Some people are genetically more prone to gum disease. This does not mean it is inevitable that you will lose your teeth. It simply means that you have to work harder than others to prevent it.
2. Puberty/Pregnancy/hormonal changes
At different times throughout a woman's life she will experience fluctuations in hormonal levels. These can make the gums more sensitive and at time react strongly to hormonal changes. For example you may notice that your gums bleed more easily at different times of the month. This sensitivity may make you more susceptible to gum disease.
3. Stress
Stress is linked to many serious conditions such as hypertension and cancer. Stress can make it more difficult for the body to fight off infection, including the infection associated with gum disease. There is increasing evidence of a link between stress and gum disease, possibly caused by the stress hormone cortisol. A person who is stressed is also less likely to take adequate care of their teeth through brushing and flossing.
4. Smoking
Smokers are more likely to get gum disease. A smoker is less likely to have his/her own teeth in later life than a non-smoker. In addition, the healing process is slower in a person who smokes, meaning that your gums will heal more slowly and less predictably than a non-smoker. This also applies if you have a tooth removed.
Mouth Reasons to Quit Smoking:
- Improve your chances of keeping your teeth for life.
- Avoid expensive and time-consuming dental treatment required to replace teeth lost due to gum disease.
- Avoid the increased risk of developing cancer of the mouth and throat, a cancer which tends to be detected late and require extensive surgery, radiotherapy and chemotherapy.
- Avoid always having an unpleasant odour from your breath.
- Your teeth will look cleaner and brighter, giving you more to smile about.
- Fillings will not discolour as quickly.
and while you're thinking about it, here are a couple of links to get you started! Quit.ie and Irish Cancer Society. Don't forget to come back to keep reading!
5. Diabetes
If you are diabetic, you are more likely to get gum disease and it may worsen more quickly than a non-diabetic. A diabetic has less resistance to infections and gum disease is one of these. Not only that, there appears to be a two-way relationship between diabetes and gum disease. Gum disease triggers the body's inflammatory response which can affect insulin sensitivity and lead to unhealthy blood sugar levels. Therefore if you are diabetic or at risk of diabetes, it is all the more important to seek help and get your gums into great condition.
6. Medication
Some medication, including anti-depressants, the oral contraceptive pill and some heart medication can affect the way your mouth works, leaving you at greater risk.
7. General Health, Poor Nutrition
A diet lacking in essential nutrients stops the body from fighting infection effectively and compromise the body's immune response. Therefore poor nutrition can worsen the condition of your gums. In recent years, evidence is also starting to emerge of a link between obesity and gum disease.
More Info: Perio is the website of the American Academy of Periodontology and contains loads of well-researched, up-to–date information about gum disease and its wider health implications.
Diagnosing Gum Disease
At every checkup we routinely examine your gums to assess your periodontal (gum) health. This consists of gently probing along the gum line with a blunt instrument.
So what are we looking for?
Does the gum bleed? Is there Plaque and Tartar present? How deep is the space (pocket) between the tooth and gum?
Possible Findings:
- No bleeding, pockets are 1-3mm deep . . . . . . well done, healthy gums!
- Bleeding, pockets are 1-3mm deep . . . . . . you have gingivitis.
- Bleeding, pockets are 3-5mm deep . . . . . . you have early periodontitis.
- Bleeding, pockets are 6+mm deep . . . . . . you have moderate-advanced periodontitis.
Most people fit in to a combination of the above categories. For example, you may have gingivitis or quite healthy gums in the areas you brush well and have periodontitis affecting more difficult to reach teeth.
Treatment of Gum Disease
We Treat:
The treatment we recommend afterwards depends on the above assessment. Sometimes you will just need a thorough scale and polish, to remove plaque, tartar and stains, coupled with a few tips on improving your oral hygiene. However, if you have signs of periodontitis or have very hard, heavy buildup of tartar below the gumline, we should undertake more intensive cleaning to remove the unhealthy material which is causing the problem. This is done by cleaning a section of teeth at a time, usually giving you some local anaesthetic to make you more comfortable. The treatment is then done over 2-4 visits, depending on your level of need. This is called subgingival debridement or root planing. In most cases, this treatment is completed by our dental hygienist, Lillian.
You Treat:
We will help you to improve your tooth-brushing technique and floss or use other interdental cleaning gadgets. This is an essential part of beating gum disease. It makes sense that inflammation caused by the daily build-up of germs will not be controlled unless it is removed daily. It can take a few months of considerable effort to improve your technique but once you get there, you will do everything with minimal effort and not consider it a chore!
We may also recommend specific mouthwashes which have ingredients suited to fighting the types of bacteria which cause gum disease. In severe cases, we may recommend an antibiotic.
Make sure to return for a Follow-Up!
This is a really important part of the treatment and unfortunately is the one that most people slip up on. Re-evaluation is an important phase of treatment for gum disease because we do not know whether treatment has worked until about three months after its completion. This is the time the gum tissues take to repair, heal and remodel. If we don't get an opportunity to do an early follow-up, we cannot assess healing. This is different to other aspects of dental treatment which involve hard tissues which do not change quickly after treatment. At your follow-up we assess healing by measuring the gum pockets and looking for signs of inflammation and make recommendations based on those findings. This might involve no treatment, a little treatment or if we are concerned that healing is not taking place, we may recommend a referral to a gum specialist (periodontist).
Back to top
Pregnancy & Child Health

There are many good reasons for taking care of your dental health before and during pregnancy. Many women have the impression that you should not have any dental treatment when you are pregnant. This is not the case. It is perfectly safe to have simple dental treatment when you are pregnant. We avoid taking xrays unless absolutely essential and we will only do emergency treatment in the third trimester, simply because it is difficult to lie back for a long period of time at that stage.
Problems which can occur during pregnancy:
- Gums can become sore and inflamed, bleeding easily. If your gums are already a little unhealthy due to the presence of plaque and tartar, hormonal changes can make that inflammation much worse. This can be minimised or avoided by making sure your gums are in great shape before you become pregnant. Even during pregnancy, attending for cleaning and improving your home care will help so if you notice more gum bleeding from an early stage, make an appointment and get the problem checked.
- Diet can be erratic and you may suffer from 'morning sickness'. Many women believe that their teeth deteriorate during pregnancy due to losing calcium- this is not correct. Regular snacking (it's ok I'm pregnant!) and nausea/vomiting will increase the acidity of the mouth, possibly leading to progression of tooth decay and acid erosion. Then the baby is born and it may take several months before you even think of making a dental appointment, resulting in a long period of time for tooth decay to worsen.
- Your options are limited if you have pain. The only painkiller which is considered safe to take during pregnancy is Paracetamol, which though it is an excellent painkiller, may not give you full relief if you develop a dental infection or nerve pain.
Overall, it makes good sense to plan ahead and have any dental treatment you may need completed before you are planning a pregnancy. It may surprise you to read that taking this action may also have a positive effect on your child's dental health. One of the risk factors for early childhood tooth decay is actually presence of tooth decay in the mother's mouth. The bacteria which cause tooth decay are transferred to the child's mouth via normal mother/baby interaction, making the child at risk of tooth decay if they receive sugary food/drinks frequently.
Please continue reading for advice on taking care of your child's teeth in the future.
Children's Dental Health
First of all, let's have a look at the normal development of your child's teeth.
Your baby will get 20 baby teeth, usually between birth and 2.5 yrs. These teeth will remain in your child's mouth for between five and eleven years. The loss of the first baby tooth and arrival of the tooth fairy is an important event in your child's life and usually happens at approx. 6 yrs age. The baby teeth are then gradually lost over the following 5-7 years.
Each baby tooth is replaced by permanent teeth which are the incisor teeth, canine teeth and premolars, 20 in total.
Around the same time your child loses his/her first baby tooth, other important teeth are appearing at the very back of the mouth. These are the first permanent molars and come up behind the baby teeth. So that adds four more teeth 24 in total.
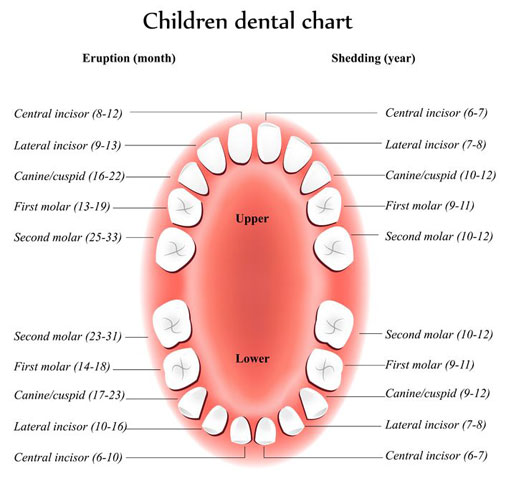
At the same time your child is losing the last of those original 20 baby teeth, at approx. 12 yrs, the second permanent molars appear behind the first permanent molar teeth, now 28 in total.
Finally, the third permanent molars (better known as wisdom teeth) appear as your child reaches adulthood.
If you took an xray of a five year old child's jaw, you would see most of the permanent teeth are already present and growing. In fact your child's permanent front teeth and first permanent molars are starting to develop at birth! It can happen that illness in early childhood can affect the enamel development of permanent teeth which appear 5 years later, resulting in a weaker surface. Similarly, the nutrition your child receives from birth contributes to the formation of the teeth they will have for life.
Why is it important to take care of my child's baby teeth?
- Maintain your child's comfort for eating and speaking from age 2-12 years.
- Prevent development of tooth decay which can cause pain and infection. In what other case would you knowingly put your child at risk of getting an infection or abscess elsewhere in the body?
- Prevent your child from needing dental treatment which can sometimes be difficult for everyone involved. It is much easier to instil a positive attitude to dental health and visiting the dentist in a child if they only require simple preventative treatments.
- Each baby tooth is maintaining space for a permanent tooth. If a baby tooth has to be removed early due to tooth decay, that space can be lost, causing a crowding problem later. So a baby tooth removal at age 5 years can cause braces at age 12 years. This is especially important for the baby teeth at the very back of the mouth.
How do I care for my child's teeth?
The main dental problem for children is tooth decay. You can read more about the prevention of decay in our Tooth Decay section.
The four key steps for children are:
1. Keep all tooth surfaces clean by brushing twice a day.
A child's teeth should be brushed from one year on. As most plaque gathers at the gumline, brushing should be directed to that area. Young children (under 8 years old) do not have the dexterity to brush effectively which means you must brush for them. After that, brushing should be supervised closely until you are confident that they have developed a great technique and don't take short-cuts! When children brush their teeth themselves, they tend not to clean difficult to reach areas, find it difficult to clean one side (same side as the hand holding the brush) and avoid the gumline where most plaque is sitting.
2. Watch the frequency of intake of sugary food and drinks.
Sugary foods are everywhere in a child's life and it can be very difficult to maintain a good routine on diet.

Drinks: As young children need frequent hydration, it is especially important that the drink they have frequently contains no sugar. This essentially means sticking to milk or water as much as possible. Juices, including diluted cordials contain some sugars and are acidic and can cause a lot of damage if your child develops a taste for them. This includes drinks which are marketed as been low in sugar. Fizzy drinks should be avoided except for a very occasional treat.
Giving a baby sugary drinks in a bottle or beaker should be avoided, especially at night-time. Very young children can develop a particular pattern of tooth decay called 'Early Childhood Decay' at aged 1-2 years if they are fed in such a way. Even frequent breast-feeding at this age, especially at night-time, can contribute to this problem. When your child goes to school, have a rule that they take water with them.
Foods: Between meals snacking should be savoury, not sugary. Treats are sweets, lollipops, chocolate, and biscuits. Pick a day or two per week that your child has a treat and stick to that. Keep the treats in a place that they cannot access them and try show good example by not eating treats in front of them. Have treats after mealtimes to reduce the frequency of eating.
Have a look at the cereals you give your child for breakfast. Some of them are very sugary and it's not just the obvious ones like Cheerios or Coco-pops. Some cereals really stick to the grooves of teeth and with pressure to get out the door to school/crèche in the morning, tooth brushing is not always optimal at this time of day. Good options are porridge, plain Ready-Brek, Weetabix, Shredded Wheat. These have less sugar and more fibre/ good quality nutrition.
3. Use fluoride in a suitable format from age 2 years on.
Fluoride toothpaste can be used from aged 2 years. Before that, the child will swallow any toothpaste which can cause problems for teeth developing at that time. After age two years, put a tiny smear of toothpaste on your child's brush and gradually increase it to a pea-sized amount as they develop good ability to spit out. Keep toothpaste out of reach so they don't eat it!
Follow the manufacturers' guidelines regarding which paste to use for different ages. To get maximum benefit from the ingredients in toothpaste, you should not get your child to rinse vigorously after brushing. Get them spit all the toothpaste out only, or rinse with a quick brush of a wet toothbrush. The toothpaste is then left on the tooth and has a chance to strengthen the surfaces. From age 6 years on, the child can also use a mouthwash. This is especially helpful if they have had tooth decay in the past. Fissure sealants are also an excellent preventative measure to protect molar teeth.
4. Take your child to the dentist for a check-up at least once per year.

Try to have a particular time of year when you get dental checkups done for your children and stick with it. This prevents a long lapse in time occurring between checkups, during which tooth decay could damage several teeth. You will receive a text message reminder when a visit is due. If your child has had recent tooth decay or has another dental issue which we need to monitor, we may recommend that you bring him/her along 6 months later. We will revert to a 12 month interval as soon as the problem is resolved.
Fissure Sealants
A high proportion of tooth decay occurs on the occlusal surfaces of teeth. This is the biting surface that we use to chew our food. This surface is covered in grooves and fissures which tend to catch plaque and food fragments. A fissure sealant is used to cover this area and protect the tooth from developing decay on this surface.
It is a simple procedure to get done. The tooth surface is first 'etched' with a gel, washed, dried and the sealant is placed carefully in liquid form onto the surface. The sealant is immediately light-cured with a bright blue light which causes it to set hard in a matter of seconds. We usually recommend sealants for the first and second permanent molar teeth, which grow into the mouth at approx. age 6 and 12 years respectively. Ideally a tooth should be sealed as soon as it has grown enough to be able to keep it dry. However, they can be done anytime after the tooth has erupted. The children who benefit most from fissure sealants are those who have had some tooth decay in the past and those with deeper fissures on their teeth.
Back to top
Teen Dental Care
Take care of your teeth in your teens and it will pay off for life. Have a look at our sections on tooth decay and tooth wear to find out a little bit more background information and then come back here.
What problems do teenagers have with their teeth?
1. Bleeding gums and smelly breath
Having healthy gums is an important part of having teeth that look good when you smile. Unhealthy gums look uneven, red and inflamed. Healthy gums do not bleed. If you notice your gums bleed when you brush or even when you eat or touch them, you probably have gingivitis. Gingivitis means 'inflammation of the gums'. This is caused by the build-up of harmful germs in your mouth due to poor tooth brushing technique. Gums with gingivitis look swollen, red and not very attractive. You may also have an unpleasant smell from your breath, noticeable to people standing close to you.
-
Think about:
- Do your gums bleed when you brush?
- Do you really make a good effort to brush your teeth or is it too quick to be thorough?
- Do you try to floss your teeth?
How is it treated? First you should get your teeth cleaned by a dentist or hygienist to remove the plaque and tartar (plaque which has hardened onto the tooth surface). After that, make a really good effort to learn how to brush your teeth well, spending time to brush every side of every tooth, concentrating along the gum-line and then use dental floss to clean between them. A soft toothbrush is best to use. Using a mouthwash is helpful but will not solve the problem unless you improve your cleaning method also. Teeth must be brushed twice a day, every day to keep gums healthy. Over a few weeks, your gums will stop bleeding, feel better, and look better.
2. Tooth Decay
Most people get most of the tooth decay they get in their whole lives during their teenage years. If you can get through your teenage years without needing much dental treatment for tooth decay, you will probably have great teeth for life. It's worth the effort to take great care of your teeth in your teens.
Thinking about what you are eating and drinking on a normal day-to–day basis and how you care for your teeth is really important here.

-
Think about:
- Do you snack alot on sugary foods between meals?
- Do you drink a lot of juices, smoothies, fizzy drinks, sports drinks?
- If you go to the shop or tuck-shop at school, do you often treat yourself to something sweet…..sweets, lollipops, bars, bubble-gum?
- Are you hit-and-miss with the way you brush your teeth?
- Do you skip flossing your teeth?
If the answer is 'yes' you are at greater risk of developing tooth decay. These are habits which you must decide to change for yourself. Nobody else can do that for you. Your dentist can nag, your parents can nag but at the end of the day, it's your problem to sort out yourself!
- Steps to take:
- Cut out the sugary junk food
- Drink mainly water (or milk)
- Don't snack too often between meals and keep it healthy. Eating three good meals every day will reduce your cravings for snacks between meals.
3. Acid Damage - Why are fizzy drinks so bad for your teeth?
Non-diet fizzy drinks are intensely sugary and all fizzy drinks, including diet drinks and sports drinks, are very acidic. As described in our section on tooth wear, acidic drinks soften the outer surface of your teeth and make them weaker and thinner. It is then easier for sugars and germs to cause tooth decay. Altogether, you end up with thin, yellow teeth and need loads of fillings…not a pretty picture!
4. Smoking - Does smoking damage my teeth?

Smoking will not cause tooth decay on its own but smoke stains stick to weak enamel very easily and can become engrained in the enamel, making them impossible to remove. Therefore you can end up with unsightly black and brown marks on your teeth. Smoking causes a lot of problems for gums. Most people who smoke develop gum disease and this can begin during your teens. It is very common for students to develop a painful gum infection which is associated with poor brushing and smoking. Smoking is also the major risk factor for development of cancer of the mouth.
5. Braces
Teenage years are the best time to have orthodontic treatment to straighten your teeth. This is because your bone is still growing so it responds quicker when teeth are moved. Facing into having a brace on your teeth for a year or two is difficult but the time flies and the result is worth the wait.
Not everyone needs braces and teeth do not have to be perfectly straight to look great and be perfectly healthy. Your dentist will advise you on whether you need a brace and refer you to an orthodontist for assessment if required.
The tips mentioned above about diet and good tooth-brushing become much more important when you are wearing a brace. The wires and metal brackets on your teeth make it much more difficult to clean your teeth well food fragments get caught very easily. This means you run the risk of developing severe tooth decay if you do not take great care of them.
Back to top
Tooth Trauma Care
Dental trauma is a very common occurrence and can have long-term consequences for the tooth/teeth involved. Even when a tooth gets a knock from which it appears to recover ok, it is still important to see your dentist for an examination of the area. This is particularly important for children.
When a child's permanent tooth grows into the mouth, it is not completely formed and is fragile. It gradually completes growing over two-three years after it first appears, ie for an upper front tooth which appears at age 6 years, it may not be fully grown until the child is 10 years old. Unfortunately, a lot of dental trauma occurs in this age group.
Teeth can be damaged in three ways when they get a knock:
- The tooth is fractured.
- The tooth is loosened or moved in its socket.
- The tooth is knocked out of the mouth.
Tooth Fracture
This can vary from a tiny piece of enamel to a large piece of the tooth.
 |
 |
| This young girl fell and fractured her front tooth while playing. | Forty minutes and five shades of composite later, it's hard to tell tooth from filling material. |
What to do?
Find the piece of tooth if you can. If it is one piece, it may be possible to rebond it to the tooth. Pop it in some milk and take it with you straight to your dentist.
The treatment needed for a fractured tooth depends on what are of the tooth is involved. If it involves the enamel and dentine layers only, we usually repair the fracture by rebonding the tooth fragment or placing a tooth-coloured composite 'tip'. Treatment is more complicated if the pulp area of the tooth is involved and a root canal treatment is usually required.
In all cases, regular monitoring is required for 6-12 months after the injury occurs. This is to keep an eye out for complications which can develop as a result of trauma. Further treatment is recommended only if necessary.
Tooth loosened
If a tooth is loosened in its socket but hasn't fallen out, push the tooth back into place with a clean finger. Then go straight to your dentist who will assess the problem.
An injury may also cause a tooth to be pushed upwards into the bone. This can cause a lot of damage as the surrounding bone and gum are crushed. Again, go to your dentist straight-away to get it checked. Leaving it a day or two can prevent the dentist from providing the best care for the tooth. This is particularly important for young children whose baby teeth are damaged as the permanent tooth is in the bone just above it and may be damaged too.
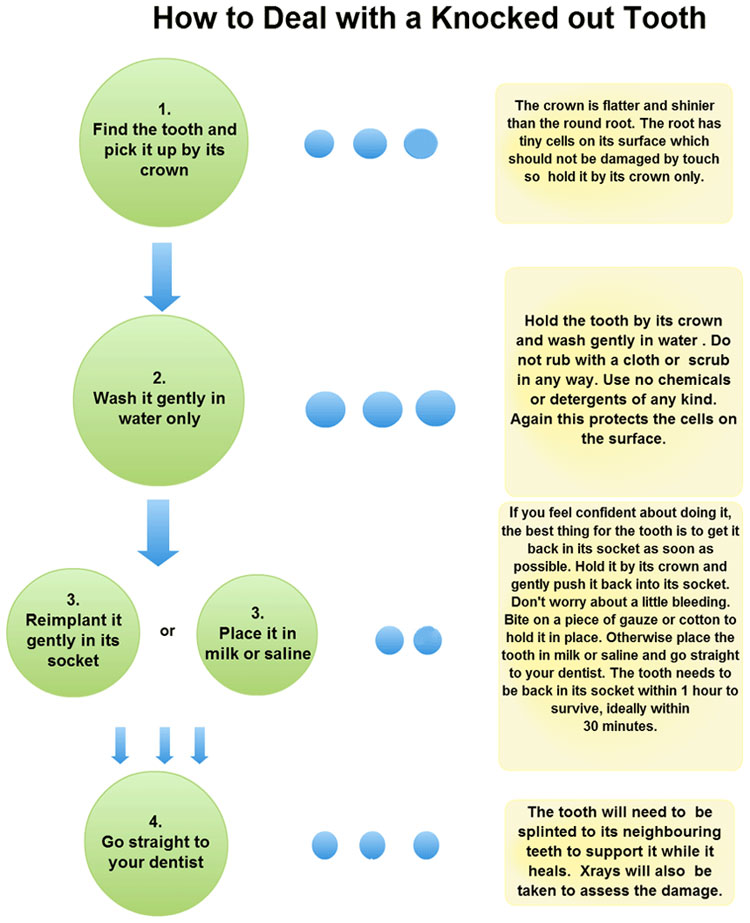
Tooth knocked out
First let's deal with baby teeth. It is recommended not to put a knocked out baby tooth back in its socket because it tends not to reattach well and can damage the permanent tooth above it.
When a permanent tooth is knocked out of its socket, it can be a dilemma for all involved. However, very specific action should be taken straightaway if the tooth is to be put back in place and heal successfully. So, take a minute to read the information below so you are familiar with the steps which should be taken.
Back to top
Tooth Removal Aftercare
Instructions after having a tooth removed
Instructions following the removal of a tooth.
- Bleeding - It is normal to have a taste of blood and some oozing from the socket after a tooth extraction. If you think it is bleeding continuously after you leave the surgery, roll a clean piece of cotton into a pad the size of your finger, place it over the socket (where the tooth was removed), sit down and bite continuously on it for twenty minutes. If it is still bleeding after this time, repeat the process. If the bleeding persists please do not hesitate to contact us.
- Pain - Some pain is to be expected after the extraction, possibly for a few days. The amount of pain experienced varies greatly. If you are uncomfortable when the numbness starts to wear off, then take a painkiller you would normally use, following the instructions on the packet. Paracetamol is a good option provided it is suitable for you.
- Local anaesthetic - Numbness can persist after an extraction for a number of hours. Be careful that you do not bite the area affected eg lip, tongue, cheek. Parents in particular should watch their child to avoid biting and causing a nasty cut. Avoid hot liquids until the numbness wears off.
- Swelling - Some swelling can be expected and may take several days to disappear. An ice-pack should be placed on the area affected and kept in place for up to 20 minutes at a time and then removed for the same period.
- Rinsing - Do not rinse your mouth until the day after the extraction as it can disturb early healing. From the day after, rinse your mouth several times per day with a generous pinch of salt dissolved in a cup of warm water. Continue for 4-5 days.
- Tooth-brushing - You should brush your teeth as normal but avoid just the socket area for a two days.
- Eating - Eat a slightly softer diet for a few days and avoid the socket area. Avoid very hot or very cold food and drink.
- Smoking - Avoid smoking completely on the day of the extraction and if possible for a few days after. Smoking delays healing significantly and smokers are at greater risk of developing a painful infection called a 'dry socket'.
- Alcohol - Avoid alcohol on the day of the extraction.
Back to top
